Wheels In
Intro + Opening Thoughts
Last week, I had the pleasure of attending the “Collaborative Summit on Health Equity and Value-Based Care,” a collaboration between Duke Orthopedics and the Duke-Margolis Institute for Health Policy. The meeting was a first of its kind effort to bring together innovative minds passionate about high-quality, cost-effective, and equitable MSK care. I thoroughly enjoyed dinner the night before where I met people from across the healthcare spectrum doing important work here. Many thanks to course co-chairs Christian Pean, MD and Erica Taylor, MD, MBA, two Duke orthopedic surgeons elevating the discourse and bringing awareness to challenges and opportunities surrounding value-based specialty care.
It was an honor to be invited to speak about a particular interest of mine: the role technology (including AI) will play in making value-based care (VBC) ortho a reality. My talk, titled “Next Generation VBC: The Evolving Role of Technology and Artificial Intelligence,” outlined the potential of technology in value-based models.
Meanwhile, I took copious notes during the day-long event, and this week’s post will highlight seven lessons I learned from an outstanding healthcare summit.
Dem Dry Bones
From the EIC’s Desk
When Christian invited me to speak at the conference, I jumped at the chance. I’m a firm believer that delivering innovation relies on synthesizing a wide range of thoughts and opinions. Events like Duke’s summit present the perfect opportunity to broaden and deepen knowledge around certain topics. Participating is a terrific way to share what you know, fill in the gaps of what you don’t know, and discover things you haven’t even considered. In that regard, the summit did not disappoint. Here’s what I learned (and what I shared).
Lesson #1: Site of Service
Directing care to an outpatient setting is a key component of value-based specialty care, especially in MSK. Migrating costly joint replacement and spine procedures to ambulatory surgery centers (ASCs) significantly reduces costs. Payers will continue to pursue mechanisms like site-of-service incentives that push care to less expensive settings. How do we take full advantage of the efficiency and savings associated with ASCs in a way that’s safe? The best approach is to implement robust processes and procedures—including tech-enabled patient engagement platforms and AI-driven data analysis—to facilitate safe care migration.
Take-home #1: Develop appropriate pathways to safely shift site of service to cost efficient ASCs.
Lesson #2: Participation
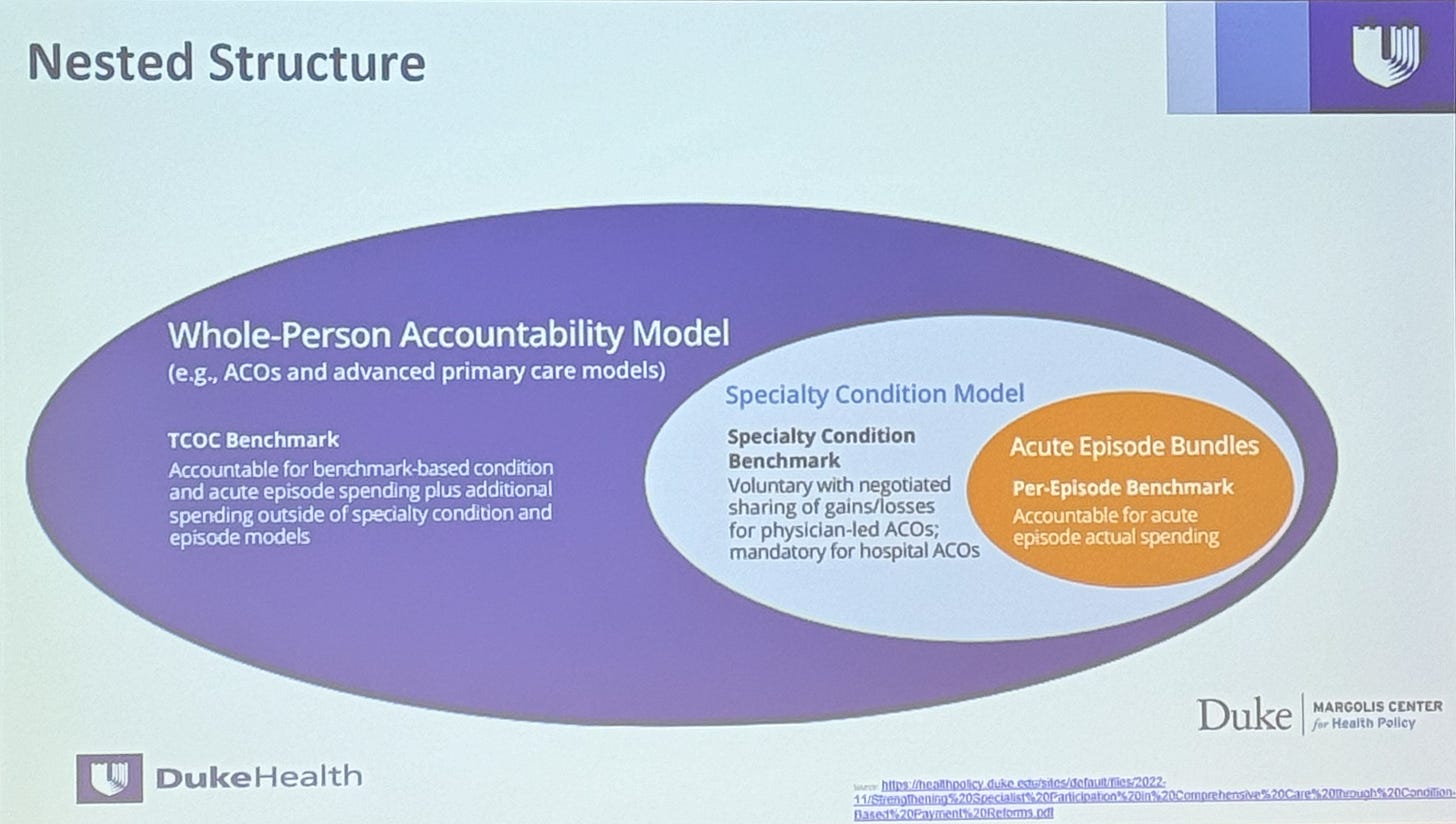
Should participation in value-based models be mandatory or voluntary? In ortho, we have both, and there’s evidence to support either approach. CJR is a mandatory program, while BPCI participation is voluntary. The argument against voluntary bundles is that low performers choose not to participate to avoid two-sided risk. However, mandating participation accelerates the transition away from fee-for-service toward VBC. Critics point out that mandatory VBC participation punishes critical-access hospitals that often care for a complex patient population. Developing more sophisticated risk stratification tools can mitigate this problem and protect health equity.
Beyond model participation rules, it’s clear that successful VBC ortho approaches must reduce care variation, leverage the use of scorecards/dashboards, and offer the ability to capture complexity. Complexity capture and proper risk-stratification were common themes throughout the meeting, rightfully so.
Take-home #2: Lack of model sophistication hinders widespread adoption. Solving this issue will be critical to the evolution and success of VBC models.
Lesson #3: Engaging Payers
Another problem to be solved: how to engage payers. When approaching insurance companies and health plans to develop a value-based partnership, data is critical. There is a spectrum of payment models that extends from traditional FFS to a host of different VBC arrangements that offer some version of capitation or shared savings. Of the value-based models, global sub-capitation has been proposed as the most effective approach. Global sub-capitation works for condition-specific VBC by incentivizing ownership of the entire care journey (for a particular patient population). It’s more robust and sophisticated than bundles tied to surgical episodes. However, global sub-cap shifts a substantial portion of risk to the care provider. Careful design and implementation are required to ensure success.
Take-home #3: You need data to engage payers. Global subcapitation, which fosters whole-person care, may be the preferred VBC approach.
Lesson #4: Creating Care Pathways
The Duke Department of Orthopaedic Surgery is doing innovative work to develop a condition-based VBC model through their Joint Health Program. Surprisingly, Duke found that only one-third of OA patients saw their primary care physician (PCP) first. The majority went straight to the orthopedic specialist. Of the patients who went to their PCP first, 80% were subsequently referred to the specialist. Only 20% of those patients ended up requiring joint replacement; the remaining 80% were managed non-surgically. Furthermore, Duke found that many specialists don’t closely adhere to evidence-based guidelines or appropriate use criteria.
This situation begs for a re-designed care model, and that’s exactly what the Duke Joint Health Program aims to do. Patients with arthritis go through a robust education process and comprehensive, whole-person evaluation (including mental health screening). Next, they’re enrolled in an all-encompassing MSK conditioning program. The entire process is coordinated and monitored by specially trained clinicians who bridge the gap between PCPs (who may not feel comfortable managing MSK conditions) and orthopedic surgeons (who may not follow established guidelines).
Frankly, I love this model. The CMS is sending strong signals through its Transforming Episode Accountability and Making Care Primary models that it wants more collaboration between primary care physicians and specialists. However, as Duke’s analysis of their MSK patient flow demonstrates, this may not be the right approach. Building the appropriate financial structure around this model is going to require time, data, and transparent collaboration between stakeholders, something that remains elusive.
Take-home #4: Successful implementation of VBC MSK requires redesigned care models and expertise that bridges the gap between primary and specialty care.
Lesson #5: The Importance of Health Equity
A clear theme from the conference: MSK outcomes are influenced by factors often underappreciated by traditional care. Social drivers of health (SDOH), including psychosocial factors and mental health, play a significant role in treatment outcomes. As part of their work, the team at Duke discovered a high prevalence of psychological distress in arthritis patients. It’s estimated that 80% of what makes up a person’s health is determined outside of the clinical setting. Socioeconomic factors, physical environment, and health behaviors all contribute. You cannot have success in value-based care without understanding and addressing these factors. Tools such as the Social Vulnerability Index (SVI) and Area Deprivation Index (ADI) can help us better understand our patients, develop sensible policies and procedures, and achieve value in a more effective way. Not all patients face these issues, but many do. Just because we don’t do a good job looking for them doesn’t mean they don’t exist.
Take-home #5: Outcomes are significantly impacted by social drivers of health. Success in value-based care requires a focus on health equity.
Lesson #6: Defining Value
You can’t have a value-based healthcare conference without attempting the impossible: defining what VBC means. It’s tempting to view value as a balance between cost and quality. In reality, these concepts are synergistic, not antagonistic. Quality care does not mean cheap care, and focusing on one does not need to come at the expense of the other. It’s OK to spend money on things that matter, if you demonstrate how and why they matter.
Again, data is key. Payers, employers, and health plans require evidence before they come to the table on specialty VBC models. That said, when presented with data, these entities should uphold their end of the bargain. Employers may be quicker to act as their incentives are more immediately aligned with high-value providers. The relationship between payers, health plans, and providers is more complex. Steerage—providing financial incentives to drive patients to preferred providers—is another mechanism to drive VBC. While it’s a powerful lever, steerage must be implemented thoughtfully and with the patient’s (not the payer’s or employer’s) best interests in mind.
Take-home #6: Cost and quality are not mutually exclusive. Defining and demonstrating value requires data.
Lesson #7: Technology + VBC
The conference generated cautious optimism about the potential of technology to facilitate scaling of MSK-focused population health. By leveraging tools such as asynchronous messaging, RPM/RTM, LLM-powered chatbots, and predictive/generative/causal AI, we can offer patients an elevated healthcare experience informed by data. Carefully implemented technology generates insights needed to realize the promise of patient-specific, personalized-care delivery. AI-powered tools enable dynamic triage, offer next generation voice agents, and provide advanced asynchronous care. Efforts like the Coalition for Health AI (CHAI) bring together “a diverse array of stakeholders to listen, learn, and collaborate to drive the development, evaluation, and appropriate use of AI in healthcare.” Cool stuff.
Technology brings with it a host of concerns that need to be addressed. These tools should be used to support doctors and patients, not to deny care or impede shared decision-making. While tech can improve access, lower barriers, and reduce biases, it can also perpetuate biases and reduce health equity. We must foster health literacy and ensure equitable access to technology while ensuring our models are trained on representative data.
Take-home #7: Technology can be the catalyst for sustainable VBC MSK care. Tech should be used to enhance care delivery, not increase barriers to care.
Small Incisions
Quick Takes on Timely Topics
This proposed bill in California could have a big impact on digital health (Second Opinion)
My Take: Few would argue against keeping bad actors out of healthcare. Some (including me) would argue that heavy-handed legislation that lacks subtlety and nuance often produces unintended consequences. If the bill stifles innovation (which these seemingly well-intentioned but often overreaching efforts do), things could be worse.
Anyone who is pushing healthcare forward in a novel, sustainable, and innovative way should be supported, not hamstrung by unsophisticated, catch-all legislation. There must be a mechanism for good actors to prove they're good actors. It's incumbent upon them to bring evidence, and it's incumbent upon decision-makers to give that evidence credence.
Absolutism, narratives, and echo chambers in healthcare discourse are counterproductive, and we'd do well to move past them. We can and must pursue any viable avenue of change if there's any hope to make progress. (Consider the amount of money spent on CMS/CMMI programs that have produced few meaningful results.)
Bad actors should be held accountable. This includes corporate backers and venture capitalists. They shouldn't be allowed to shrug or feign ignorance when their companies misbehave. They should be subject to the same penalties levied on wayward clinicians when things go sideways.
(Side note: Where is the legislation that addresses the underlying causes of consolidation? Where are the efforts to support physician-led healthcare?)
Verily, Alphabet health company, to enter GLP-1 obesity market (Stat News)
My Take: Big Tech is still searching for its sweet spot in healthcare. Apple scrapped the idea to roll out its own health clinics. Google Health is no more. Amazon Care (in-person) became Amazon Clinic (virtual). Verily’s Lightpath initiative (an evolution of portco Onduo) has features of specialty value-based care with a focus on diabetes. There’s RPM/RTM, AI assistants, and coordinated chronic care management that aims to synthesize disparate data sources. GLP-1s hold a lot of promise, and Verily is not alone in trying to leverage them as part of a broader effort. Companies like Ro and WeightWatchers have also cast their lots with these meds. It’s a crowded market. Can Verily offer something others can’t? The company needs a win following its recent reorganization and pivot away from moonshots to more financially viable efforts.
Leaked documents reveal patient safety issues at Amazon’s One Medical (Washington Post)
My Take: Medical call centers are difficult to run, and One Medical certainly can improve its processes. However, the bigger story here is that being customer obsessed in healthcare is different than being customer obsessed in retail. Not that the goal isn't always to deliver a wonderful experience. The difference is that running a successful healthcare business and finding bottom line ROI on high-touch care delivery is hard. One Medical could offer these things when in growth mode and using venture capital money. But when it's time to check the bottom line, these things are often the first to go.
Why Walgreens’ US Health President Is ‘Bullish’ on the Role of Retail in Healthcare (MedCity News)
My Take: It’s hard to parse where retailers really stand in healthcare. Walmart execs made bullish statements shortly before shuttering all Walmart Health clinics. Walgreens’s “bullish” stance towards the role of retail in medicine belies its own struggles with VillageMD. I agree with Mary Langowski that consumers (patients if you will) want ease and convenience. In my mind, the right approach is to advance traditional care models. I suspect retail health struggles because healthcare is more relationship and trust based than people realize. A transactional approach works OK for low-acuity problems but less so for longitudinal, chronic care.
CMMI’s savings record sparks concern among lawmakers (Healthcare Dive)
My Take: Like an unfazed young quarterback who keeps firing it downfield despite a spate of interceptions, CMMI keeps tossing around VBC models hoping something will connect. I'm certain that, given fair incentives, a meaningful voice, and an equal seat at the table, healthcare innovators can design sustainable VBC programs. But there needs to be more collaboration and a willingness to listen and engage. Otherwise, you're just slowly adding to the alphabet soup of also-ran programs.
The Gold Standard
Polling the Crowd
The Light Box
Healthcare Visuals

From the Gallery
Amplifying Community Voices
"Policy is finally aligning with incentives for more equitable care models. We need to run with the data on cost and area deprivation indices, incorporating social drivers of health into specialty care. Despite numerous studies highlighting disparities, we need proof that equity-focused incentives can achieve cost containment and quality improvement. AI will play a huge role in scaling these models. At Duke, we aim to lead in leveraging technology for sustainable and equitable population health in orthopedics. I hope this summit is just the beginning and we spark more innovation and action in value-based care." — Dr. Christian Pean, MD, MS
A unique summit like this is extremely valuable and was made successful by the intentional variety of expertise in the room. A key predictor of sustainability of equity initiatives is the level of connection people feel to the overall mission. Without a doubt, evaluating trends in technology, health markets, and clinical operations through the lens of health equity achieves this goal. It is critical that these innovative ideas don’t remain in form of promises, but rather that they are realized and translated to actual practice. This conference balanced innovation with practical implementation strategies to aid in adoption and sustainable engagement. The reality is that this work benefits ALL of us and we are dedicated to building avenues for collaboration across our enterprise and beyond. I am thankful for the authentic commitment of the faculty leaders to improving the care experience for our patients, our teams, and our communities. — Erica Taylor, MD MBA
Wheels Out
Signing Off and Looking Ahead
I thoroughly enjoyed my trip to Durham. The meeting represents a jumping off point for weaving together value, equity, and technology into a novel approach. Multiple conversations I had at the meeting left me feeling that we are close to realizing the potential of VBC MSK. There is a growing willingness to embrace value-based specialty care and collaborate to design sustainable, effective models. The opportunity to innovate has never been greater. Change is afoot.
Until next time,
Ben Schwartz, MD, MBA
Editor-in-Chief / Senior Clinical Fellow