Prologue
In just 12 months, Commons Clinic flipped the script on orthopedics—and now it’s ready to do the same for all specialty care.
Last year, Commons made a bold claim—it could kill a health system in 5 easy steps. Simply take everything broken about traditional healthcare and turn it on its head. The approach? Build the world’s first consumer-focused, value-based multi-specialty clinic with a strong ambulatory component and smart implementation of technology.
Easy.
To test that thesis, Commons launched a next-generation MSK specialty practice in one of the toughest healthcare markets—Los Angeles. In partnership with high-quality orthopedic surgeons, the company successfully negotiated risk-bearing contracts with multiple payers and invested $9.75 million in an advanced musculoskeletal ASC. Commons’ one-of-a-kind Orthopedic Center of Excellence achieved > 3x YOY growth while delivering high-value, state-of-the-art, patient-focused Orthopedic care.
Thesis proven. Health systems on notice.
Backed by a validated specialty care model and a $26 million Series B round led by RA Capital, Commons Clinic is now operationalizing its next phase of growth—expanding into multi-specialty care through its new Wholebody platform.
This week’s edition of The Surgeon’s Record discusses how Commons successfully leveraged MSK as its specialty care test case and how the company is building the foundation of next-generation multi-specialty care.
This is Commons Clinic 2.0.
Executive Summary
Commons Clinic is building the first integrated specialty care platform rooted in diagnostics, proactive intervention, and whole-person care. This post introduces the next chapter:
The Product: The Wholebody Assessment—a multi-system diagnostic that identifies emerging health risks through advanced imaging, labs, and functional testing
The Model: Wholebody Specialty Care—longitudinal specialty care guided by early detection and seamless procedural intervention
The Platform: Commons = Wholebody Specialty Care—a system where diagnostics feed tightly into Centers of Excellence, enabling rapid, coordinated action
The Outcome: A reimagined specialty care system—lightweight, connected, and built for the modern patient
Proving the Model: The MSK Test Case
You have to start somewhere.
As the top of the funnel and gatekeeper to specialists, care delivery innovation has typically centered on primary care. There are many so-called “Alternative/Advanced Primary Care” models, including concierge/subscription-based models (One Medical), ACOs (Aledade), and Medicare Advantage-centric provider groups (Oak Street Health).
These models achieve varying degrees of success when it comes to improving costs and outcomes. None of them offers an elegant solution for handling downstream specialty care referrals. Instead, capitation incentivizes them to avoid specialists or patients are farmed out to external networks when specialty care is necessary.
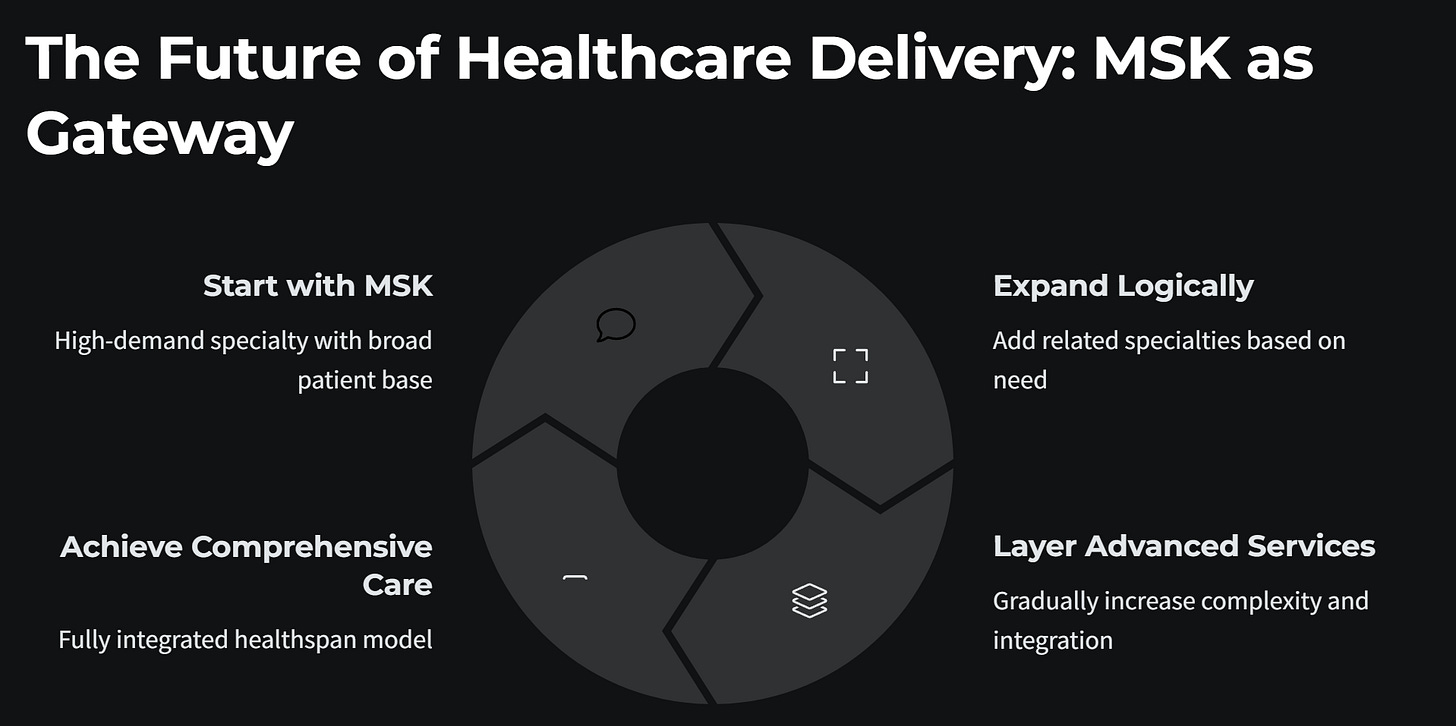
Commons Clinic opted for a different approach—start with specialty care and work backwards. Instead of avoiding specialty care, intervene earlier and smarter. With its high utilization rates, significant systemic costs, and variability in care quality, orthopedics was a natural place to start.
MSK is a crowded space, with one important caveat. Well-known companies like Hinge Health and Sword Health are virtual MSK companies whose core competency is tech-enabled PT sessions. Much of their ROI stems from surgical avoidance. As such, these are not true care delivery companies capable of guiding patients through the entire MSK care journey.
Nothing against Hinge or Sword—both have achieved significant milestones. But Commons is a specialty care provider, not a virtual MSK competitor.
Commons Clinic was built on the principle of holistic care. From the outset, the goal was to offer a comprehensive, value-focused MSK solution. Commons now boasts 17 top-notch physicians in a competitive major metropolitan market (LA), contracts with Aetna, Blue Shield, and Carrum Health, a Spine Surgery and Joint Replacement ASC (MOSI), and a newly opened state-of-the art clinic with on-site physical therapy.
To date, Commons Clinic’s traction and progress in orthopedics have exceeded expectations. But MSK was always intended to be the starting point for greater ambitions, not the endgame. The Commons vision is, and has always been, to create a new system—reimagined multi-specialty care with prevention, early detection, and enhanced care coordination at its core.
Commons Clinic 2.0 takes lessons learned from MSK to build the foundation for next-generation multi-specialty care.
Building the Foundation of Multi-Specialty Care
Commons 2.0 broadens the MSK approach to encompass prevention, early detection, and specialty care services across all body systems. Simply put, Commons Clinic is building the nation’s leading Specialty Care Practice—the Mayo or Cleveland Clinic for modern healthcare. This initiative positions Commons Clinic as the first integrated, holistic specialty care provider, seamlessly coordinating elite, high-value care across disciplines to optimize patient health.
What’s unique about this approach?
Care model innovation isn’t new. Alternative primary care (APC), advanced practice models (APMs), accountable care organizations (ACOs), and CMS/CMMI value-based programs all attempted to usher in a new era of cost-conscious, quality-focused care.
The results are middling. This recent analysis from Avalere Health paints a sobering picture—most VBC models fail to appreciably save money or improve outcomes. Many rely on turning PCPs into gatekeepers, avoiding or delaying specialty care and retrofitting solutions onto the chassis of a broken system.
Commons Clinic 2.0 overcomes these challenges by rethinking the relationship between primary and specialty care and redefining what “healthspan” truly means. Traditional healthcare is reactive—prevention, early detection, and a holistic view of health are afterthoughts. They should be key features.
That changes with Commons 2.0—Wholebody Specialty Care.
Instead of struggling with chronic care management, primary care becomes what it’s intended to be: the first and last stop on the patient care journey. By coordinating, navigating, and aggregating all aspects of care, Commons 2.0 ensures timely interventions and seamless care transitions. Specialty care isn’t avoided or unnecessarily delayed, it’s accelerated—when clinical necessity demands it.
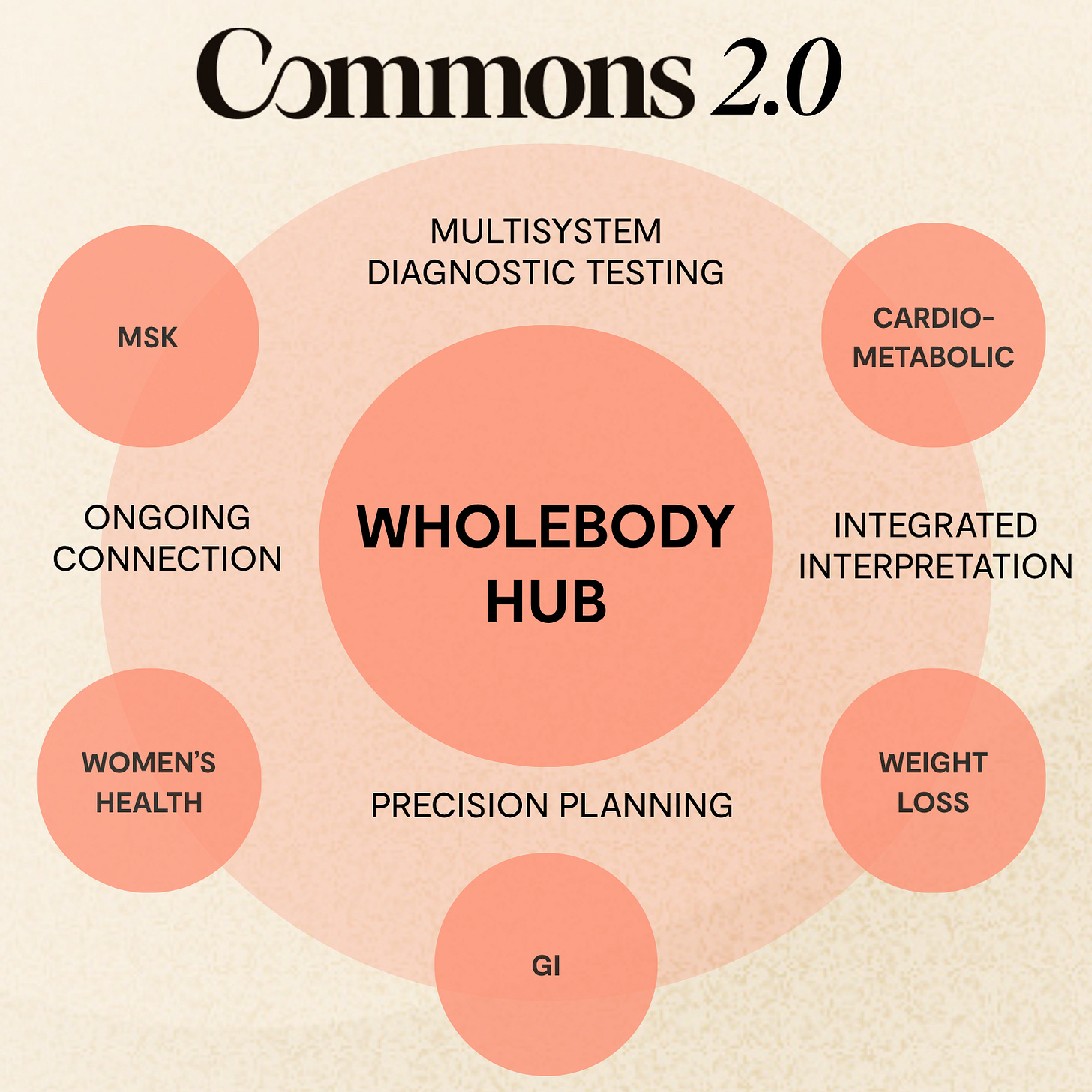
Commons 2.0 Core Components
Along with a comprehensive history and physical, Commons 2.0 incorporates four core components into an evolved approach:
Multisystem Diagnostic Testing: State-of-the-art tools like GRAIL’s Galleri multi-cancer early detection test, Cleerly’s AI-powered cardiac insights, and continuous biometric monitoring to power early detection and risk profiling. These technologies allow Commons to shift from reactive treatment to proactive intervention.
Integrated Clinical Interpretation: A multi-disciplinary care team—including physicians, nutritionists, physical therapists, and nurses—reviewing findings together and collaborating in real time.
Precision Planning: Results and recommendations are shared in a detailed report and discussed during a follow-up consultation with a physician. Insights are translated into action, and each patient is given a clear care plan with tightly integrated specialty referrals as indicated.
Ongoing Connection: Continual, supportive care provided through post-assessment “check-ins”, referrals, or therapy sessions based on an individual’s clinical pathway needs. Closing the care loop enables longitudinal care and health maintenance.
At the center of this new model is Commons’ flagship diagnostic offering: The Wholebody Assessment—a tech-enabled entry point into the broader Wholebody Specialty Care platform.
More Than Longevity and Wellness
The Wholebody Assessment isn’t concierge wellness with a nicer lobby or an executive physical wrapped in AI-generated formatting. What we’re building is something entirely different—true system redesign.
Our core demographic is in their mid-to-late 50s, a group often overlooked by traditional care models. They’re not young biohackers chasing longevity and focused on avoiding catastrophic care. And they’re not Medicare patients navigating complex chronic conditions.
Our patients are in their prime intervention window—still active, still working, and often facing the first serious signs of cardiovascular, metabolic, orthopedic, or oncologic disease.
This population doesn’t need vague wellness plans or lab services tied to another app. They need a clear, data-driven pathway to intervention—integrated diagnostics, early specialist evaluation, and tightly coordinated care that turns insights into meaningful action.
That’s exactly what The Wholebody Assessment delivers.
A collaborative team approach. A foundation of multisystem data. A focus on timely, personalized, specialty-level care—before the catastrophic event, not after. We're not selling peace of mind. We're offering precision-driven action for people who are ready to take control of their health.
The pillars of the program—Cardiometabolic, MSK, Women’s Health, Weight Management, GI, and Preventive Oncology—form the foundation of a novel multi-specialty model. The Wholebody Assessment isn’t a once-a-year physical. It’s the mechanism by which Commons Clinic will turn comprehensive body-system data into end-to-end care pathways and specialty service lines.
Actionable insights only make sense when they lead to action. Wholebody does just that.
Rails to the Future: Specialty Service Line Expansion
With MSK proven and the holistic care model established, the next step is building out specialty care service lines. Board-certified cardiologist Dr. Jenica Ortega now leads the Wholebody program, with a specific focus on building the cardiac, metabolic, bariatric, and women's health service lines. Additionally, former CEO of The Oncology Institute, Brad Hively, has joined Commons' board to advise on specialty value-based care strategy and expansion.
Imagine Wholebody as Grand Central Station, gathering and synthesizing important clinical information, then efficiently placing patients on high-yield care pathways—i.e., the system's rails. At the end of each rail sits a Commons micro-Center of Excellence—a purpose-built ASC or OBL that provides high-quality procedural and surgical care with seamless clinical integration. These micro-COEs don't just close the loop on care—they create a virtuous cycle of detection, treatment, and long-term maintenance.
No fragmentation. No silos. No delayed care.
Wholebody isn't just surfacing problems. It's solving them—efficiently, holistically, and in-house. From blood draw to biopsy, scan to stent—Commons 2.0 closes the loop.
Case Example
John Smith is a 55-year-old busy executive. He travels a lot for work, exercises when possible (though not regularly), and has a diet dominated by airport lounge food and restaurant business dinners. He has a family history of cardiac disease—his father experienced a heart attack at age 60 that required stenting and, eventually, heart bypass surgery.
Mr. Smith enters Commons Clinic’s Wholebody program and undergoes the most detailed medical evaluation he’s ever had. Given his family history and present health status, Mr. Smith is placed on a tailored Cardiometabolic pathway (railway) including comprehensive lab work, a coronary artery calcium scan, and VO2 max testing. Not surprisingly, the evaluation reveals a few areas of concern. But, instead of simply pointing out problems and leaving Mr. Smith to figure it out for himself, the Commons approach turns these insights into tightly coordinated actions.
Mr. Smith immediately proceeds along the cardiometabolic pathway, leaving the central care hub to travel to the next node—a Cardiac Micro-Center of Excellence—where he meets with a team of experienced, high-quality cardiac specialists. A state-of-the-art workup reveals coronary artery disease, leading to cardiac catheterization and stent placement. A potential heart attack is prevented, and everything is covered through a Cardiac Care Bundle Program.
His cardiac specialty care completed, Mr. Smith rides the care rail back to the central care hub, where the Commons 2.0 care team takes over. Seamless communication and integration ensure Mr. Smith remains on plan, improves his cardiometabolic health, and avoids future health problems.
Prevention + Early Detection —> Timely Specialist Evaluation + Intervention —> Longitudinal Maintenance + Monitoring
Specialty care as it should be.
Commons 2.0: A Blueprint for Wholebody Specialty Care
Imagine multiple care railways— MSK, Cardiometabolic, Women’s Health, Weight Loss, GI, and more—originating from a central hub of advanced preventive and diagnostic whole-person care to high-quality specialty care nodes and back. Holistic, light-weight, efficient, and clinically superior. Comprehensive evaluation, early detection, and actionable insights turned into meaningful interventions.
Wholebody = Specialty care evolved—the essence of Commons 2.0.
This vision isn’t a pipe dream. It’s happening now. Commons Clinic has already proven its model works through its success in delivering value-focused orthopedic care. With Series B funding complete and the Wholebody platform launching, the next phase is taking lessons learned from that model to create the foundation of a better system.
The time is now.





This sounds interesting and similar to what our team has discussed. Start from specialty care, not primary care in order to re-imagine healthcare. I come from a Health Information Technology perspective. Does Commons Clinic have a centralized hub where all the data from all the patient's different providers is collected so that all of whole body issues are known to each clinician treating the patient? If so, How is that data structured? FHIR? OpenEHR? or a proprietary EHR data standard? If not, is that on your roadmap? Thanks.
Would love to build health plans around this.