Decentralized and Distributed: The "Hub-and-Spoke" Model
I’ve often railed against the moratorium on physician-owned hospitals (POHs) included in the Affordable Care Act. While the ACA didn’t outright ban POHs, it rendered them financially untenable by blocking Medicare and Medicaid reimbursement.
The move wasn’t some evidence-based policy masterstroke — legislators simply caved to lobbying pressure from hospitals and health systems. Now, 15 years later, we have more consolidation, skyrocketing healthcare prices, and a worsening doctor shortage. Who would have guessed? Apparently, not policymakers. (Workweek did an excellent job breaking it all down here).
While there is increasing talk of reviving POHs, is the debate still relevant today? Shifting healthcare trends suggest it might not be. Consider the following:
Migration to ambulatory surgical centers and outpatient facilities
Technology solutions that enable remote care, continuous monitoring, and hybrid approaches
Hospital at home, reduced utilization of post-acute settings, aging in place
Prevention, longevity, and holistic health
Consumerism, commoditization, and healthcare marketplaces
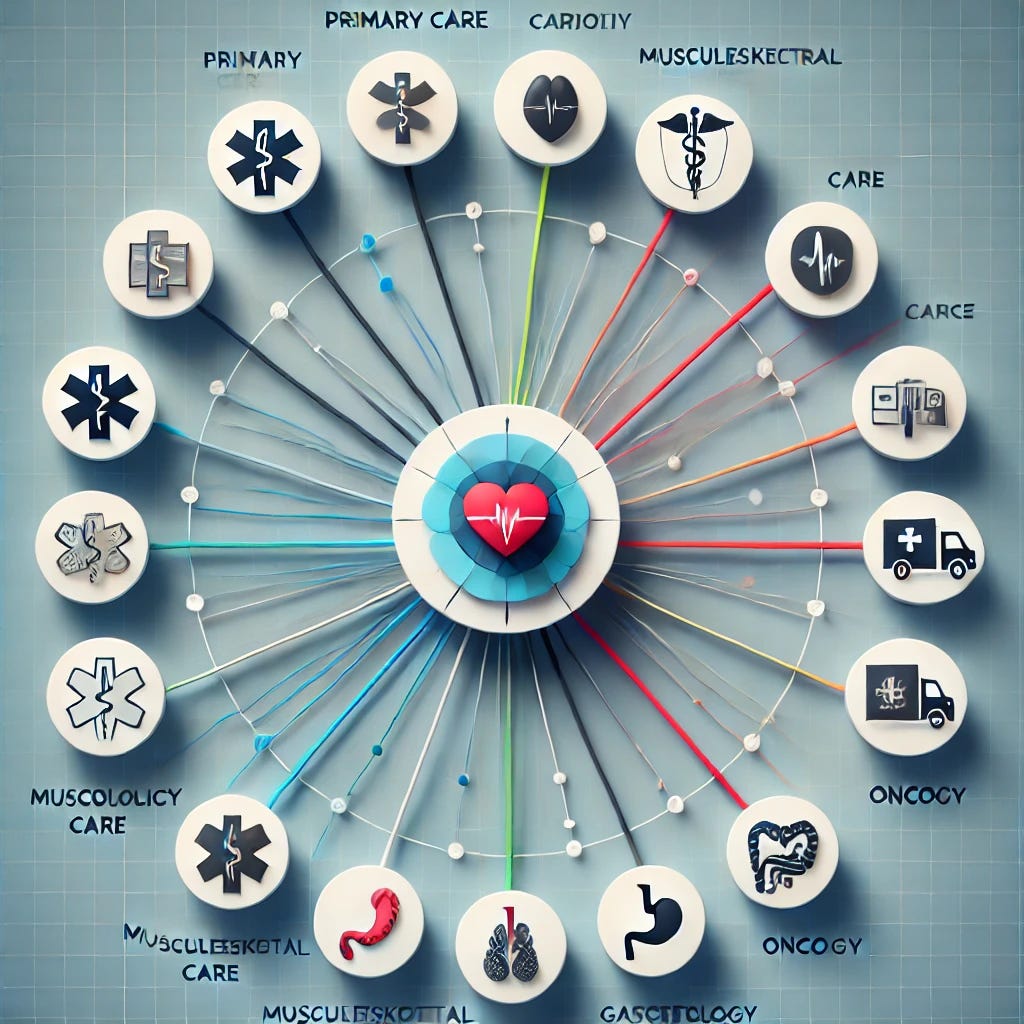
The common thread? A future no longer dominated by complex, inefficient, expensive systems. These trends suggest that next-generation care will be decentralized and distributed — offering high-value, integrated care without the bureaucracy, inefficiency, and cost of legacy health systems. It will follow a hub-and-spoke model where primary care serves as “Grand Central Station,” and specialty services are organized into micro-Centers of Excellence.
What does such a model look like? First, let’s consider what it means for a system to be decentralized and distributed.
Decentralized and Distributed Systems: An Overview
The concept of “decentralized, distributed” systems became popular during the rise of blockchain and Web3. The grift and hype that tainted these use cases shouldn’t sour our discussion. When applied thoughtfully to healthcare, these concepts make a lot of sense.
Centralized healthcare is represented by traditional health systems — large, bureaucratic, and complex. In contrast, a decentralized and distributed model resembles an elite group of smaller, specialized centers working in concert—each excellent in its niche but collectively greater than the sum of its parts.
(The following discussion was adopted and adapted from this excellent, detailed article).
Decentralized Systems
“Decentralized systems are…architectures where multiple nodes, often spread across different locations, share control…without a single central authority. Each node in a decentralized system operates independently but collaborates with others to achieve common goals. This structure enhances fault tolerance, scalability, and resilience compared to centralized systems.”
Many aspects of decentralized systems are attractive in healthcare:
No single point of failure. Resiliency. Scalability. Load distribution. Coordination and communication. Enhanced reliability. Who wouldn't want these things from their healthcare system? Now let’s consider what distribution adds to our model.
Distributed Systems
“Distributed systems are…architectures where multiple independent nodes...work together to achieve a common goal. These nodes communicate and coordinate with each other…appearing as a single coherent system to the end user. Distributed systems aim to improve performance, reliability, scalability, and resource sharing by leveraging the collective power of interconnect[ivity].”
While decentralization ensures local autonomy, innovation, and responsiveness, distribution adds geographic coverage, resource sharing, and transparency. These are coveted characteristics of a highly functioning healthcare system. But how do we put it all together to design something sensible and viable?
Decentralization and distribution aren’t just abstract tech concepts, they're the key to solving inefficiencies, cutting costs, and improving patient outcomes. Applying these principles to healthcare involves a ‘hub-and-spoke’ model built around primary care hubs and micro-Centers of Excellence (COEs).
The Hub and Spoke Model
The Hub - Preventative & Maintenance Primary Care
In this model, primary care is the central hub, focused on prevention, maintenance, and wellness. It coordinates, navigates, and aggregates all aspects of patient care, ensuring timely interventions and seamless care transitions.
This approach improves patients’ access to basic health services and health education. It emphasizes early detection and management of common health issues, reducing the downstream burden on specialty care services.
At the same time, PCPs aren’t forced outside their comfort zones — incentivized to practice specialty-level care by “value-based” capitation. By leveraging primary care as the aggregator of patient data and steward of whole-person health, the hub-and-spoke model ensures that patients receive appropriate, timely care.
Primary care functions as it was always intended, supporting holistic health and wellness through patient engagement — not drowning in a sea of complex chronic care management. When necessary, PCP hubs frictionlessly navigate patients to the spokes — high-value specialty centers.
The Spokes - Specialty-Driven Micro Centers of Excellence
Micro-Centers of Excellence form the spokes of our model — specifically Ambulatory Surgical Center/Office-Based Laboratory (ASC-OBL) hybrids. ASC/OBLs perform a mix of office-based E&M, diagnostic services, interventional procedures, and ambulatory surgeries under one roof. They excel at delivering comprehensive specialty care in an efficient and cost-effective manner.
Each micro-COE operates with focused expertise in musculoskeletal, cardiovascular, endocrine, and other specialties. They streamline patient pathways, improve procedural efficiency, and reduce costs compared to hospital-based interventions. Micro-COEs are masters of their trade, capable of treating all but the highest acuity patients. Executed well, these centers obviate the need for POHs, instead leaning into the trend toward smaller, more focused outpatient centers.
Not only do spokes integrate seamlessly with hubs, but they’re also in constant communication with each other, distributing and decentralizing knowledge and resources across a greater care network. Information flows freely, ensuring each center has the most up-to-date information. System redundancy and transparency create “checks-and-balances” that reduce errors and allow for constant improvement through iteration.
Finally, spokes are distributed across a geographical area, ensuring that care is local, accessible, and aligned with community needs. Using a lightweight model, micro-COE ABS/OBL hybrids are easily scalable, responding quickly to changing demands while remaining malleable and at the forefront of treatments. Eventually, “hive mind” data collection and analysis across the network identifies trends and tailors treatment for personalized, high-impact care.
While this model may seem similar to existing clinically integrated networks, even well-regarded CINs like Kaiser and Intermountain have struggled with operational bloat, restricted patient choice, and slow responsiveness to change. Their ‘integration’ often creates as many silos as it removes.
Here’s how our model’s different.
CINs — Evolved
Unlike other CINs that rely on top-down, administratively dense, centralized structures, ASC-OBL hybrids maintain autonomy at the local level. Traditional CINs cover a broad range of services, but their complex structures create inefficiencies and fragmented patient care. They often aren’t as integrated as they seem and frequently challenge patients to navigate their opaque processes. Other healthcare innovators have tried to cobble together their own version of a CIN. But if you don’t directly manage the entire process, you’re not really integrated.
ASC-OBL hybrids are highly focused on specialty care while ensuring streamlined workflows and superior patient outcomes. Primary care hubs, freed of the burden of trying to be jacks of all trades, become masters of integration and synthesis. They achieve holistic care with a true emphasis on health and wellness. At the same time, they ensure access to specialty care when needed.
Through decentralization and distribution, the hub and spoke model significantly reduces administrative overhead and infrastructure costs. It offers intrinsic value through transparency, high-level expertise, and proven outcomes. Micro-COEs are lean and ultra-efficient, reducing waste and passing savings to payors and (most importantly) patients. Where CINs are slow to act, ASC-OBLs are flexible, allowing for rapid adoption of innovative technologies, constant iteration, and process improvement while challenging the status quo.
Finally, this model empowers doctors and engages patients. It hides complexity from end users who enjoy a patient- and physician-friendly model of care. Clinicians operate with greater autonomy and have true ownership. Care delivery aligns with patient needs rather than institutional politics and spurious quality metrics. Distribution brings care closer to patients, while decentralization offers an engaging experience tailored to specific community needs.
Why It Works
Executed properly, this approach makes the idealized healthcare system a reality. Here’s why it works:
The Hub: Preventative and Maintenance Primary Care – Primary care serves as the central hub, focusing on prevention, maintenance, and wellness. It coordinates, navigates, and aggregates all aspects of patient care, ensuring timely interventions and seamless care transitions.
The Spokes: Micro Centers of Excellence (COEs) as Specialty Extensions – ASC-OBL hybrids act as the spokes, delivering highly specialized, procedure-driven care that extends beyond traditional hospital settings. Each micro-COE operates with focused expertise in musculoskeletal, cardiovascular, endocrine, oncology, and other medical specialties.
Optimized Patient Flow – Primary care, as the aggregator of patient data and the driver of proactive decision-making, improves care coordination and navigation. The hub-and-spoke model ensures that patients receive the highest-value care in the most integrated fashion.
Quality-Driven Outcomes, Enhanced Patient Experience – This model reduces fragmentation, eliminates unnecessary hospital visits, and provides a patient-centric pathway that is both cost-effective and high-quality. Specialists in micro-COEs refine and perfect diagnosis and treatment, improving patient outcomes through repetition, focused expertise, and distributed knowledge.
Cost Reduction + Value Creation — By emphasizing health, wellness, and prevention through primary care, the model becomes a true “well care” system. At the same time, specialized centers deliver expert “sick care” when patients need it. Creating synergy between the hub and spokes eliminates low-value care and waste while improving outcomes. Value becomes a byproduct of the process, not a fruitless carrot-and-stick exercise.
Decreased Health System Dependence — By managing most conditions in outpatient settings, hospitals are reserved for emergencies and highly complex cases, improving system-wide efficiency. (Editor’s Note: Legacy hospitals and health systems would quickly cry foul here — but that’s a topic for a different post).
Scalability and Adaptability — Once established, the model’s framework can be expanded across regions and specialties, allowing for tailored implementation based on local healthcare demands. Shared resources, economies of scale, and distributed knowledge mesh with equity, access, and flexibility. The hub-and-spoke model creates a constantly evolving system of best practices while understanding that healthcare is local.
How to Pay for It
What about financials? Discussion around healthcare innovation always comes back to how you’re going to pay for it — a conundrum few have been able to solve. Here are some possibilities:
Public Funding + Regulatory Support: With a new focus on efficiency, CMS/CMMI should establish pilot programs and grants for innovative care models. Legislative advocacy will be crucial to ensuring favorable reimbursement policies. This includes eliminating or paring back Certificate of Need laws, Stark regulations, and the Anti-Kickback Statute.
Private Investment: Private equity, venture capital, and public-private partnerships can provide the necessary capital for scaling ASC-OBL models. Serious healthcare investors should be drawn to the cost-effectiveness and efficiency of decentralized care models. The catch — this is not a “pump and dump” or arbitrage opportunity. The time horizon will be measured in decades, not years.
Condition-Specific Bundles, Capitation, & Global Subcapitation: Implementing bundled payments for specific conditions allows models to receive a single payment for an entire episode of care, incentivizing efficiency and quality. Prepaid models where providers receive fixed per-member-per-month payments encourage cost-effective, proactive care management.
Evolved Value-Based Care: Engaging in contracts that tie reimbursement to quality metrics, cost savings, and patient outcomes ensures financial sustainability — with a caveat: payment cannot be subject to unfair ratchet mechanisms, and the model cannot be a victim of its own success. VBC may simply be a tweaked version of FFS that embraces transparency of cost and outcomes.
Cash Pay & Direct Contracting: Offering transparent cash prices or partnering directly with employers for specialty care packages enhances revenue while reducing administrative burdens. Subscription models could offer access to basic care with a la carte pricing for add-on services.
HSA + Stop-Loss Models: Patients using Health Savings Accounts (HSAs) paired with stop-loss insurance can self-fund care at ASC-OBL centers, ensuring access to high-quality services while managing financial risk.
Decentralized, distributed care delivery represents the future of healthcare. Combining these models creates a resilient, scalable, and patient-centered system. The proposed model restores primary care to its intended function — serving as the central hub of health and wellness. Through ASC/OBL hybrids, specialty care exists in micro-Centers of Excellence — efficient, innovative, high-quality facilities that form the spokes of our model.
This model offers venture capitalists, private equity investors, healthcare innovators, doctors, and payors a unique opportunity to invest in and shape the next generation of healthcare. Building this model won’t happen overnight, but if executed correctly, the decentralized, distributed hub-and-spoke approach achieves what has so far escaped our grasp: truly innovative care delivery.






This is a very well-written cogent analysis! The variance is in how the hub-spoke model gets executed. I am working on implementing that business model.